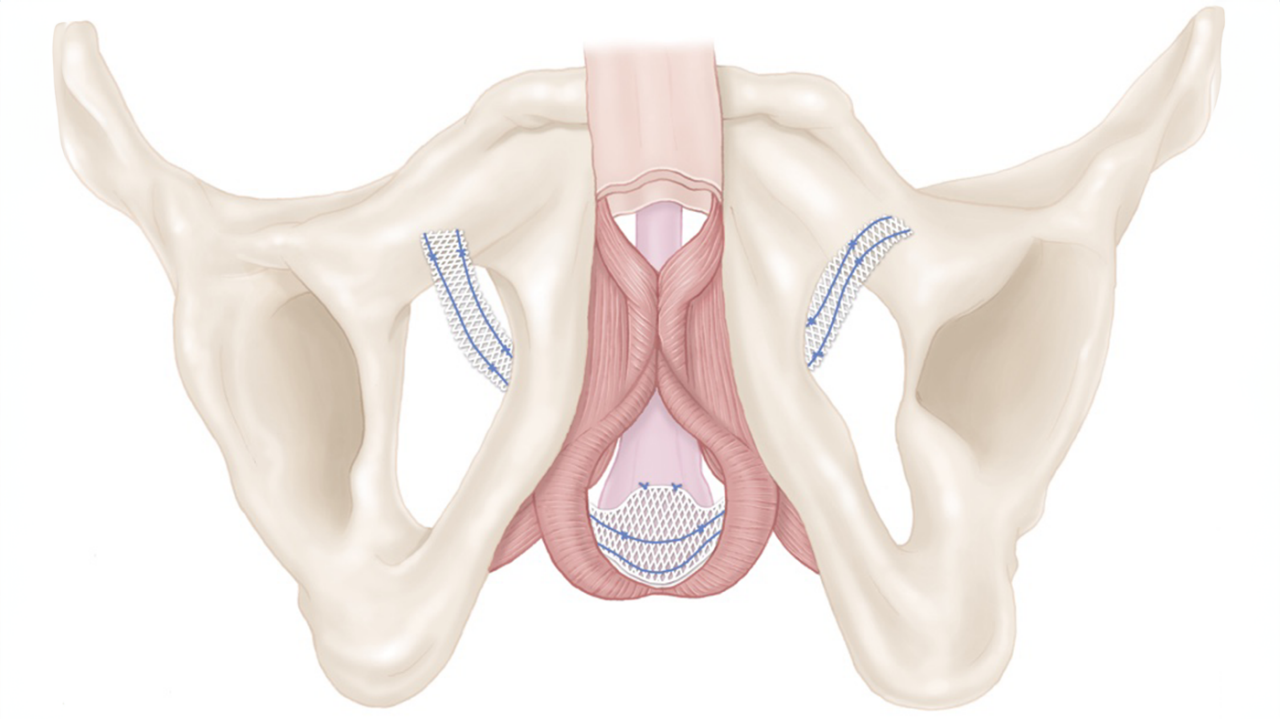
How it works
The AMS 800 System from Boston Scientific is filled with saline and uses the fluid to open and close the cuff surrounding the urethra. When you need to urinate, you squeeze and release the pump in the scrotum several times to remove fluid from the cuff. When the cuff is empty, urine can flow out of the bladder. The cuff automatically refills in a few minutes, squeezing the urethra closed to restore bladder control.